Medicina de precizie este un model de practica medicala care presupune adaptarea ingrijirilor medicale oferite nevoilor fiecarui pacient in parte. Bazat pe un diagnostic acurat care de obicei integreaza datele clinice, biologice, imagistice in contextul genetic al pacientului, medical curant poate lua o decizie terapeutica personalizata, adaptata nevoilor specifice pacientului in cauza.
Un astfel de exemplu este cel al pacientului prezentat in cadrul Congresului European de Preventie Cardiovasculara 2022. Este vorba de un tanar de 30 de ani care s-a prezentat in clinica noastra pentru un consult cardiologic preventiv intrucat analizele de rutina au indicat un profil lipidic modificat (cu o valoare marcat crescuta a LDL colesterolului si o valoare scazuta a HDL colesterolului). Analizele suplimentare au ridicat suspiciunea unei boli de depozit a esterilor de colesterol, diagnostic confirmat ulterior si prin testare genetica. Astfel a fost dovedit ca pacientul nu sufera de hipercolesterolemie poligenica ci de o boala rara cu o incidenta aproximativa de 1 din 300.000 de persoane: deficit de lipaza acida lizozomala. Implicatiile acestui diagnostic sunt semnificative din punct de vedere al tratamentului. Daca in hipercolesterolemia poligenica prima linie de tratament pentru controlul hipercolesterolemiei o reprezinta administrarea de statine, in cazul pacientului nostru prima linie de tratament o reprezinta administrarea enzimei deficitare (sebelipase alpha).
In clipa de fata clinica noastra, impreuna cu departamentul de Genetica medicala si boli rare a UMF Timisoara si medici din sectia de gastro-enterologie a spitalului Judetan Timisoara, are in urmarire 3 pacienti cu acest diagnostic. Deocamdata tratamentul cu Sebelipase alpha nu este disponibil pe program national in Romania, iar pacientii nu il pot cumpara, pretul fiind prohibitiv (cateva zeci de mii de euro lunar). Pentru acesti pacienti s-a obtinut acordul firmei producatoare care va dona tratamentul necesar pana la introducerea tratamentului gratuit in Romania, si sunt in desfasurare demersurile legale necesare pentru ca tratamentul sa poata fi administrat in Romania.
Pentru mai multe detalii, accesați mai jos prezentarea integrală.
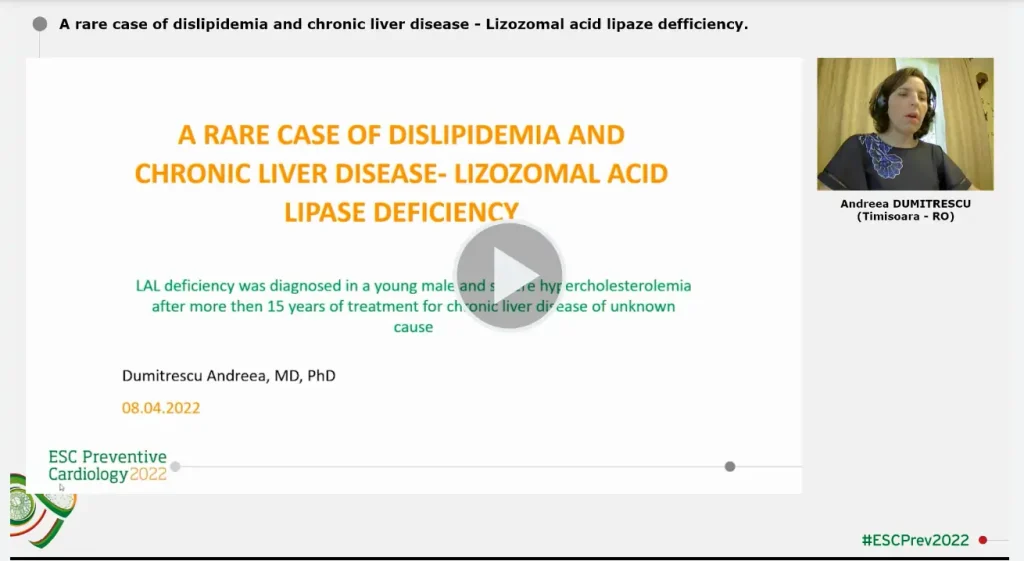
A RARE CASE OF DISLIPIDEMIA AND CHRONIC LIVER DISEASE- LIZOZOMAL ACID LIPASE DEFICIENCY
LEARNING OUTCOMES
In any young adult, a lipid profile which is not quite consistent with familial hypercholesterolemia showing low HDL cholesterol levels and high triglyceride levels combined with very high LDL cholesterol levels especially if it is associated with nonalcoholic fatty liver disease and splenomegaly should raise the suspicion of glycogen storage disease. The lysosomal acid lipase activity in plasma is a facile test for further refining the diagnosis. Ultimately the diagnosis should be confirmed with genetic testing.
CLINICAL CASE DESCRIPTION:
We present the case of a young 29 years old male patient who presented in our clinic for a preventive cardiovascular evaluation. He was diagnosed with type 2a dyslipidemia and fatty liver disease at 10 years of and has been on intermittent statin treatment. His lab evaluation showed increased LDL cholesterol, low HDL cholesterol, high triglycerides levels as well as high ALT, AST and bilirubin levels. The patient was referred to genetic testing which identified one pathogenic variant and one variant of unknown significance in LIPA (c.894G>A- heterozygous; c.416T>G (p.Phe139Cys)- heterozygous). His lysosomal acid lipase activity in plasma was 0. With a combination of 20 mg rosuvastatin and 10 mg ezetimibe daily we obtained a 50% lowering of his LDL cholesterol. For the moment this is the only LAL deficiency case presented in Romania.
PATIENT PRESENTATION
We present the case of a young 29 years old male patient who presented in our clinic for a preventive cardiovascular evaluation. He has been diagnosed with type 2a dyslipidemia and fatty liver disease at 10 years of age after the death of his father (at 29 years of age due to an ischemic stroke). At that point his lab test showed a high cholesterol level of 385 mg/dl, high triglyceride level (200 mg/dl) associated with high transaminases (ALAT=89 U/l and ASAT=95U/l). After excluding other causes of hepatic cytolysis (screening negative for infectious hepatitis B, C, E, D, CMV, mononucleosis, autoimmune diseases, normal cupper levels), hepatic biopsy was performed. The result was nonspecific showing mild stellar fibrosis, large size hepatocytes with clear cytoplasm and no inflammatory infiltrate, raising the suspicion of some storage disease. Low dose statin treatment was started (atorvastatin 10 mg/day) with a slight biological improvement (cholesterol levels decreased to 241 mg/dl) but with an increase liver transaminase level. This reaction was interpreted as a side effect of statin treatment, and treatment was stopped at 12 years of age. The patient remained without any treatment/or evaluation until his presentation in our clinic. At presentation, his physical evaluation was within normal range, his lab evaluation showed increased LDL cholesterol, low HDL cholesterol, high triglycerides levels (LDL cholesterol= 372 mg/dl, HDL cholesterol= 38 mg/dl, triglycerides= 150 mg/dl) as well as high aspartate aminotransferase, alanine aminotransferase and bilirubin levels (AST=46 UI/l; ALT=100UI/l, total bilirubin=4,17 mg/dl; direct bilirubin=0,69 mg/dl).
INITIAL WORKUP
At the presentation in our clinic the patient was asymptomatic and wasn’t following any medication. As we mentioned earlier his physical findings were in within the normal range, but we noted that his father died at 29 years of age. The cause of death was ischemic stroke in a previously healthy individual, but medical records are unavailable. Our patient’s initial lab evaluation showed increased LDL cholesterol, low HDL cholesterol, high triglycerides levels (LDL cholesterol= 372 mg/dl, HDL cholesterol=38 mg/dl, TG=150 mg/dl) as well as high aspartate aminotransferase, alanin aminotransferase and bilirubin levels (AST=46 UI/l; ALT=100UI/l, total bilirubin=4,17 mg/dl; direct bilirubin=0,69 mg/dl) and mild thrombocytopenia (138.000/mmc). His resting ECG was normal, with no signs of myocardial ischemia. Cardiac ultrasound revealed no pathological findings. Carotid ultrasound showed bilateral subclinical atherosclerosis with small partially calcified atherosclerotic plaques at the origin of both internal carotid arteries, with no hemodynamic significance. We performed an exercise ECG which showed no signs of myocardial ischemia. Abdominal ultrasound showed hepatomegaly with moderate steatosis and a mild splenomegaly. His echo elastography (FibroScan) evaluation showed a grade F2 fibrosis (stiffness 8.1 KPa). We measured our patient’s lisosomal acid lipase activity in plasma and it turned out to be 0. At this point the patient was referred to genetic testing. The genetic testing identified one pathogenic variant and one variant of uncertain significance in LIPA gene (c.894G>A- heterozygous; c.416T>G (p.Phe139Cys)- heterozygous). Subsequently genetic testing was performed on the mother of our patient (as she is the only first degree relative of the patient) and we found that she is a heterozygous carrier of an uncertain significance variant in LIPA gene (c.416T>G (p.Phe139Cys).
DIAGNOSIS AND MANAGEMENT
Based on the lysosomal acid lipase (LAL) activity and on the genetic testing, the diagnosis of LAL deficiency in our patient is quite clear. LAL deficiency is a rare genetic disorder with an autosomal recessive transmission and a prevalence of 1 in 300.000 individuals. It is characterized by accumulation of cholesteryl esters and triglycerides in hepatocytes and macrophages throughout the body. Based on the residual activity of LAL, the disease has two main phenotypes: Wolman’s disease and cholesterol ester storage disease. Wolman’s disease is the more severe form of the disease, death usually occurring in the first year of life. Cholesterol ester storage disease is the late onset phenotype with symptoms starting in childhood or early adulthood. Due to high cholesterol level it can be misdiagnosed as familial hypercholesterolemia (FH), as it happened in our patient. While in FH there is an isolated increased LDL cholesterol level, in LAL deficiency the increased LDL cholesterol level is associated with very low HDL cholesterol and high triglycerides. Associated hepato-splenomegaly should raise the suspicion of some kind of cholesterol storage disease. In our patient lipid lowering treatment was started with low dose rosuvastatin (10 mg/day). After 1 month treatment LDL cholesterol levels decreased to 221 mg/dl. At the same time a slight decrease in transaminase and bilirubin levels were observed (AST=48 U/l, ALT= 89 U/l, total bilirubin=2,44 mg/dl). The statin dose was increased to 20 mg/day. After another month his LDL cholesterol level dropped to 176 mg/dl, without any changes in his liver analysis status. We changed lipid modifying treatment to a combination of 20 mg rosuvastatin and 10 mg ezetimibe, and after another month his LDL cholesterol level was 107 mg/dl (corresponding to amore 50% lowering of LDL cholesterol). Enzyme replacement therapy with sebelipase alpha was taken into consideration, but for the moment this treatment is unavailable in our country.
FOLLOW-UP
The outcome of LDL deficiency patients is determined by the progression of the hepatic disease on one hand and the occurrence of atherosclerotic events of the other hand. Standard treatment for these patients should include the administration of human recombinant sebelipase alpha as enzyme replacement therapy. The ARISE (Acid Lipase Replacement Investigating Safety and Efficacy) trial showed in these patients a marked improvement of the mean levels of ALT, AST, LDL cholesterol, HDL cholesterol and triglycerides after 20 weeks of treatment. Unfortunately in Romania this treatment is not available. Thus, we aim to improve our patient’s prognosis by properly managing his cardiovascular risk. At this point, we obtained a more then 50% reduction of his LDL cholesterol level (from 372 mg/dl to 107 mg/dl) by using a combination of 20 mg rosuvastatin and 10 mg ezetimibe daily. Still, this level is approximately double of the 55 mg/dl target for LDL cholesterol. For further lowering LDL cholesterol levels we can either increase the statin dose to a maximum of 40 mg rosuvastatin daily or we can add a PCSK9 inhibitor to his lipid lowering treatment. Statin treatment should be carefully monitored in LDL deficiency patients. A clinical review of 12 statin treated LAL deficiency patients using hepatic biopsy showed a more rapid progression of the liver abnormalities then prior to statin treatment. After one year of treatment, our patient is scheduled for a transient liver elastography (Fibro Scan) and a liver biopsy. Hematopoietic stem cell transplantation and liver transplantation have been used in some patients with LAL deficiency and progressive liver disease but with high mortality and mixed results.
CONCLUSIONS
Although LAL deficiency is a genetic disorder, it can remain undiagnosed until adult hood. Any lipid profile showing very high LDL cholesterol, very low HDL cholesterol and high triglycerides should raise the suspicion of LAL deficiency, especially if it is combined with high transaminases and hepatosplenomegaly. Determining LAL activity in plasma is a facile test for the diagnostic. Ultimately LAL deficiency should be confirmed by genetic testing.